Prescribing Procedures for Sexual Health Nurse Practitioner
Introduction
The author has worked in Sexual health Department for the past 14 years and is currently employed as a nurse practitioner. The practitioner role entails working autonomously: taking accurate clinical histories, physical examinations, gains differential diagnosis & organises a plan of care. This plan of care often includes prescribing medications. It is increasingly becoming a necessity therefore in many specialist & autonomous nursing roles to become a Nurse Medical Prescriber (NMP) who will script the prescribing medication.
The Nursing and Midwifery Council (NMC) (2018) states that only qualified NMPs, who has successfully completed the non–medical prescribing course, may write a prescription.
The aim of this essay is to discuss the prescribing that took place for a patient that presented with genital ulcers in the Sexual Health Clinic. This essay is structured by applying the prescribing pyramid to aid practice (NPC, 1999) & adhering to the first principle, considered to be a holistic assessment.
The essay will also demonstrate an evidence-based approach to practicing as a safe independent prescriber. This can be achieved by presenting and analysing a prescribing scenario of a patient encountered within a known area of practice of Sexual Health.
The case study used is based on a female patient Katy who attended for treatment of recurrence of Herpes Simplex Virus (HSV). While this essay has been written from the perspective of a prescriber, in reality the prescription issued for this consultation was written by a qualified prescriber. To maintain confidentiality, in line with the code of professional conduct, throughout this essay, all names of patients, clinicians, hospital and all community trusts have been changed as per (NMC 2018).
This prescribing practice essay applies the Gibbs Model (1988). The author finds the model fits well with the seven principles of good prescribing and has been selected as it is something the author is familiar with and has used before.
Consider the patient
A full history was taken from Katy which included presenting complaint (PC) and history presenting complaint (HPC) including sexual history. The patient confirmed no changes in sexual history since her last attendance. A full medical, social and drug history, medication currently being taken, including herbal remedies, over the counter medicines and any known allergies was established. Open ended questions were posed by means of the patient being able to “tell her story”, for example, “what brings you to the clinic” (Peat, 2001). Closed questions were also asked, as suggested by Young et al (2009); these are helpful questions in gaining specific information related to the initial information given. For example if the patient mentions he/she have pain, an appropriate closed question would be “where is the pain?”.
It is Important for the NMP to have insight knowledge of signs and symptoms of possible differential diagnosis and be able to rule out red flags. In this case the following differential diagnosis & red flags for Syphilis chancroid & Bechet Syndrome were already ruled out. The patient received a negative syphilis blood test and negative Chlamydia and Gonorrhoea swab, followed by an examination of genital sores that showed no consistency with Behcet’s. There is no test that can determine definitively whether it is Behcet’s disease; therefore the diagnosis is primarily dependant on signs and symptoms. (British Association of Sexual Health & HIV BASHH 2015).
History revealed Katy had recurrent genital sores. Upon examination there was obvious Herpetic lesions consistent with HSV. Young et al (2009) states a sound history is an essential component of the assessment process and is vital to ensure safe practice and for the prescribing process. The diagnosis of Herpes was previously performed through Polymerase chain reaction (PCR) Wald A, et al (2003) from the affected area of skin. In this case no test or further investigations were carried out; this was because on examination the Ulcers were herpetic looking, with associated raised inguinal lymph glands. Therefore once the initial diagnosis of HSV is made, the NMP must be able recognise a recurrence HSV on clinical symptoms and thorough consultation using the Calgary-Cambridge guide to medical interview consultation model. This subsequently prevents unnecessary repeated expensive PCR tests. As previously stated, no further testing were required as the patient was previously diagnosed with HSV2 (Local Policy NHS TRUST 2018).
Strategy
Medical ethics is a system of moral principles that apply values to the practice of clinical medicine & in scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. Beauchamp and Childress (2008) developed the four principles of health care ethics.
This includes:
- Principle of respect for autonomy,
- Principle of non-maleficence,
- Principle of beneficence,
- Principle of justice.
These principles have been applied to aid and explore all of the available options to treat Katy.
Herpes Simplex Virus (HSV)
BASHH, (2015) Herpes simplex is the name given to two viruses in a family of herpes viruses. All of them, once caught, lay dormant in the body. The two viruses that cause genital herpes are: Herpes simplex virus type 1 & 2. Both types can cause symptoms on the genitals (genital herpes), the face (facial cold sores), or the hand or finger (called a herpetic whitlow) depending on where they are caught. Genetically HSV 1& 2 are slightly different but cause similar symptoms. Either can be caught anywhere on the body:
- Type 1 is more likely to reappear when it is caught on the face and is less likely to recur when it is caught on the genitals.
- Type 2 is more likely to recur when it has been caught on the genitals.
There is no difference in the visible symptoms caused by the two types, so it is only possible to establish which type you have caught through a laboratory test (BASHH 2015).
Autonomy
The patient should be provided with sufficient information such that he/she can decide on the appropriate management of their sexually transmitted infection.
When deliberating on treatment, it is important to bear in mind that other treatment options should be considered before writing a prescription; Katy was informed of the treatment options that were available. Katy also explored the option of not having any medication as, previously, the Herpes healed without treatment. But Katy was also aware that if she did not consider treatment she may have another attack. The NMP explained given that Katy had four Herpes outbreaks it would be beneficial to commence treatment; Patel et al (2015) states that treatment initiated early in an episode is most likely to be effective, as treatment prior to the development of papules is of greatest benefit. WHO (2016) guidelines recommend a suppressive therapy over episodic therapy & reassessment after one year for adults with severe recurrent clinical episodes (e.g. 4–6 times a year or more) or that cause distress due to an genital HSV infection. Taking into account the recurrence history & the distress this causes Katy, the NMP agreed with the patient that treatment would be appropriate.
Katy was provided with all the information that was required to decide on an appropriate course of action. The NMP also discussed the pros & cons along with the possible side effects of each treated option. In practice service users are given information from the BASHH (2015) guidelines, also the local policy which is accessed via the NHS intranet. Furthermore Katy was encouraged to refer to the patient information leaflet for Herpes which is in the medication box and the leaflet that was provided.
Beneficence
Patient with few recurrences may be best managed with episodic antiviral therapy or no therapy, whereas those with more frequent recurrences may find suppressive therapy more beneficial. Medical indicators considered when evaluating the potential suitability for suppressive therapy are the frequency, duration, severity and psychological impact of recurrences (BASHH 2015).
Katy discussed the number of recurrences & how this had an effect on her relationships. Katy expressed the interest in starting the suppressive treatment based on the number of herpes attack & how this had an impact on her personal life including relationships self-esteem and the stigma attached to it.
The relationship with the patient in terms of patient partnership in deciding best options is very important, having their options & views listened to & taken into consideration is important. This as a result can lead to better outcomes. The NMP reiterated information around Herpes, how there is no cure for genital herpes. However Katy was informed the treatments can relieve the symptoms. However, the medication given can decrease pain & shorten healing time (Patel et al, 2015). It can also decrease the number of outbreaks. Drugs such as aciclovir, valaciclovir, famciclovir, are a few medications given to treat the symptoms of herpes; these options were discussed with Katy.
Non maleficence
Although it was agreed to treat Katy the NMP took into consideration all the possible contraindications for the patient to commence the suppressive treatment as evidenced by the SPC (2019). Long treatment of Aciclovir is not recommended. In prolonged or repeated courses of aciclovir in severely immune-compromised individuals. In this case it may result in the selection of virus strains with reduced sensitivity, which may not respond to continued aciclovir treatment.
While the SPC (2019) suggests there are contraindications with long term use of aciclovir, the patient was not immune-compromised. Therefore there was no indication why it was not appropriate, due to safety, for the patient to commence this treatment. Nevertheless the risks and benefits should be carefully considered by the NMP, although ultimately the patient must decide whether the benefits outweigh the risks before consenting to a treatment.
Justice
The treatment for Herpes is complex, long and careful consideration or discussion with patient is important. aciclovir, valociclovir and famciclovir are the three preferred method of treatment according to the Local policy and BASHH guidelines (2014).
All options were discussed with the patient; the NMP decided that aciclovir 400 mg tablets twice daily for 3 months-6 months would be the choice of treatment; this was based on the BASHH (2014) & NHS local guidelines (2018). Further reasons for the choice of aciclovir are discussed below.
Consider choice of product
The NMP needs to take into consideration a few aspects when considering choice of treatment, very well summarised by the use of a Mnemonic EASE. (Prescribing Nurse Bulletin 1999).
- How effective is the product;
- Is it appropriate for this patient;
- How safe is it;
- Is the prescription cost effective.
The recommended treatment for adults with recurrent clinical episodes of genital HSV infection that is frequent, severe or cause distress, BASHH (2014) suggests aciclovir, valaciclovir and famciclovir for suppressive therapy. Recommended regimens are as follows:
• Aciclovir 400 mg orally twice daily;
• Valaciclovir 500 mg orally once daily;
• Famciclovir 250 mg orally twice daily.
The NMP looked at the following evidence & this is what the findings were to support the decision to treat Katy with aciclovir. Gupta (2004) suggest all three treatments for Herpes to be equally effective. Valaciclovir, Famciclovir & Aciclovir are highly effective in suppressing the frequency and quantity of genital HSV shedding, Gupta et al (2004). A systematic review & clinical trial data on the efficacy of these treatments was supported by Lincoln & Goldmen (2016) & all three were seen to be as effective as the other.
Oral aciclovir, valaciclovir, & famciclovir reduce the duration and severity of recurrent genital herpes (Patel, 2015). The reduction in duration is a median of 1–2 days. Head-to-head studies show no advantage of one therapy over another or the advantage of extended 5-day treatment over short-course therapy. Prodrugs (such as valaciclovir and famciclovir) offer simplified twice-a-day dosing.
Aborted lesions have been documented in up to a third of patients with early treatment according to Wagenlehner (2016). Patient-initiated treatment started early in an episode is most likely to be effective, as treatment prior to the development of papules is of greatest benefit. Short-course therapies offer more convenient and cost-effective strategies for managing genital herpes episodically & should be regarded as first-line options. aciclovir, valaciclovir, and famciclovir all reduce the severity and duration of episodes, (BASHH, 2015).
Literature review also showed that patients who have taken part in trials of suppressive therapy have had to have at least six recurrences per annum. Such patients have fewer or no episodes on suppressive therapy. Patients with lower rates of recurrence will probably also have fewer recurrences with treatment (BASHH 2015). Patients should be given full information on the advantages and disadvantages of suppressive therapy. The decision to start suppressive therapy is a subjective one, balancing the frequency of recurrence with the cost and inconvenience of treatment.
Patients suffering from psychological morbidity for which the diagnosis causes significant anxiety may benefit from suppressive therapy. Patient safety and resistance data for long-term suppressive therapy with aciclovir now extends to over 20 years of continuous surveillance. Patel et al (2015) confirms that aciclovir is an extremely safe compound requiring no monitoring in previously well patients & only a dose adjustment in those with severe renal disease.
The following evidence was looked at & these findings were used to support the decision to use aciclovir. Treatment for Herpes is complex and divided into primary, episodic and suppressive. This was also guided by the BASHH (2014) and local NHS policy 2014. This aids the prescriber in choosing the correct medication, dose, route and duration for the specific conditions.
Individuals who have frequent recurrences, severe symptoms or episodes which cause distress will likely choose suppressive therapy over episodic therapy. To determine frequency or severity, episodes can be monitored for the first few months. Although the benefits of the medicines may be similar, the costs of valaciclovir and famciclovir are higher than aciclovir, & therefore aciclovir is preferred method of choice in the clinic.
The practitioner did not initially contemplate cost, but from a cost effective point of view, the Table below shows the relative cost of antiviral drugs used to treat BASHH (2015).

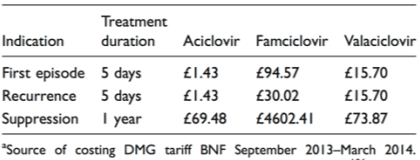
From the table we can see that if a patient is on suppressive treatment, this may become a cost burden to the clinic. NMP recognises that treatment should not be based on cost only. Due to financial constraints and local guidelines aciclovir is first line treatment. & NHS local guidelines 2018).
Negotiate a contract
When prescribing medicine to the patient Royal Pharmaceutical society (2016) requires that the patients consent and adherence with treatment must be considered. This is a shared contract which requires negotiation between the NMP & patient, Prescribing Bulletin (1999). The NMP discussed the option of not having treatment versus treatment; Katy confirmed she would prefer to take the treatment, given the recurrences she had over the past year. Allowing Katy to participate in the decision of her treatment means she is in control and as a result helps with adherence NICE (2016).
Dose and duration were then also clarified and the importance of taking the medication as prescribed & to complete the full course. On reflection, by discussing & deciding on the best treatment together this would hopefully promote concordance. Negotiating with patients & agreeing on a management plan is very important aspect of reaching patient centred care (Neighbour, 2005).
After receiving all treatment options available including benefits & possible side effects the patient agreed to start suppressive treatment aciclovir 400mg bd for duration of 3 months. The patient was given information on how to take the medicine & potential side effects.
Review
Katy was advised to return to the clinic in 6 weeks’ as per Local guidelines. Furthermore Katy was also advised to return or see her GP if symptoms worsened or did not improve after completion of treatment. NMP reiterated if symptoms occurred, to seek medical assistance early so that treatment could begin as soon as possible to reduce the risk of severe outbreaks and complications (BASHH 2015).
Record keeping
The consultation, examination findings & treatment were recorded on the electronic patient record (EPR) system as per local policy & the Code: Professional standards of practice & behaviour for nurses & midwives (NMC 2015). The records are accessible by the multidisciplinary team. The RCN (2018) States that good record keeping compiles a complete record of the patient’s/client’s journey through other services. It also allows to enable continuity of care for the patient/client both within and between services.
Reflection
The Gibbs (1988) model of reflection was applied; this allows the NMP to re-evaluate what went well, & what could have gone better during the consultation. The NMP is reasonably competent in history taking process; nonetheless the NMP felt the consultation took too long. The reason for this was the NMP being new to prescribing process it was crucial not to miss anything out. The decision to treat or not to treat was also daunting. For the patient this possibly was too long for them to be in the clinic, but on a professional point of view it allows the NMP to make sure they have written everything clearly and concisely.
This essay has focused on Katy treatment for HSV. The NMP is confident that the rationale for prescribing aciclovir was justified although initially the NMP felt a little pressure of only being able to prescribe aciclovir as first line treatment on the basis it was cheaper. Initially the NMP was unable to appreciate this, but this has now allowed the NMP to base decisions with an open mind together with sound comprehensive local & national guidelines to be able to decide on a choice of medications.
This essay has enabled the NMP to appreciate the benefits of nurse prescribing to both patient and nurse. The NMP recognises safe evidence based decisions should be made. NMP are accountable for their actions and must ensure that any decisions made cause no harm to the patient.
References
- Bickley, L. (2008) Bates Guide to Physical Examination and History Taking. 6th Ed. London: Lippincott, Williams and Wilkins.
-
Beauchamp T.L, Childress, J.F (2009). Principles of biomedical ethics. 6
th
ed New York: Oxford University Press - British National Formulary: No.76 (September 2018-March 2019) London:Pharmaceutical Press
- ahl, R. (2004). Charlie and the chocolate factory. 6th ed New York: Knopf.
- Department of Health. (1989) Report of the Advisory Group on Nurse Prescribing. The Crown Report). London: HMSO
- Department of Health. (1999) Review Of Prescribing, Supply And Administration Of Medicines. (The Crown Report Two) London: HMSO.
- Department of Health. (2006) Medicines Matters. London: HMSO
- Gupta R, Wald A, Krantz E, Selke S, Warren T, Vargas-Cortes M, Miller G, Corey L (2004)
-
Valacyclovir and Acyclovir for Suppression of Shedding of Herpes Simplex Virus in the Genital Tract
The Journal of Infectious Diseases,
Vol 190, (8), Available from
www.jid.oxfordjournals.org
[Accessed Dec 2018] - Gupta R, Warren T, Wald A. (2007) Genital herpes. Lancet London England. [PubMed][Accessed Dec 2018]
- Patel.R, et al (2014) UK national guideline for the management of anogenital herpes
- International Journal of STD & AIDS
- Miserocchi, E. Modorati G, Galli L, Rama P. (2007) .Efficacy of valacyclovir vs acyclovir for the prevention of recurrent herpes simplex virus eye disease: a pilot study.
- Nursing & Midwifery council,Standards of proficiency for nurse and midwife prescribers, Nurse and midwife prescribers. Accessed 14th December 2018
- (NMC) 2018 Nursing & Midwifery council https://www.nmc.org.uk/standards/code
- The Code Professional standards of practice and behaviour for nurses, midwives and nursing associates. Accessed 14th December 2018
- National Prescribing Centre(1999) Signposts for Prescribing Nurses – General Principles of Good Prescribing. Prescribing Nurse Bulletin. (1): 1-4.
- Neighbour, R. (2005) The Inner Consultation. How to Develop an Effective and Intuitive Consulting Style. 2nd Ed. Oxford: Oxford-Radcliffe.
- Nursing and Midwifery Council (2006) Standards of Proficiency for Nurse and Midwife prescribers. London: Nursing and Midwifery Council.
- Peat, I. (2001). How to take a sexual health history. Practice Nursing [online]. 12, (8).
- Available from: magonlinelibrary.com [Accessed January 2019].
- Pendleton, D. Schofield, T. Tate, P. Havelock, P. (1984) The Consultation: An Approach to Learning and Teaching. Oxford: Oxford University Press.
-
Royal College of Nursing Record keeping
http://rcnhca.org.uk/top-page-001/record-keeping/
[Accessed December 2018] - Silverman, J. Kurtz, S. Draper, J. (2005) Skills for Communicating with Patients. 2ND Ed. Oxford: Radcliffe.
- Wald A, Huang M-L, Carrell D, et al. Polymerase chain reaction for detection of herpes simplex virus (HSV) DNA on mucosal surfaces: comparison with HSV isolation in cell culture. J Infect Dis 2003; 188: 1345–3151.
- Wagenlehner FM, Brockmeyer NH, Discher T, Friese K, Wichelhaus TA. The presentation, diagnosis and treatment of sexually transmitted infections. Dtsch Arztebl Int. 2016;113:11–23. [PMC free article] [PubMed]
- Workowski K. Sexually Transmitted Diseases Treatment Guidelines, 2015. . 2015 Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6403a1.htm. Accessed 19 December 2004. [PMC free article] [PubMed]
- Young, K. Duggan, L. Franklin, P. (2009) Effective Consulting and History-Taking Skills for Prescribing Practice. British Journal of Nursing. (18) 17: 1056-1061.
- Young, K. Duggan, L. Franklin, P. (2009) Effective Consulting and History-Taking Skills for Prescribing Practice. British Journal of Nursing. (18) 17: 1056-1061.

 PLACE THIS ORDER OR A SIMILAR ORDER WITH ALL NURSING ASSIGNMENTS TODAY AND GET AN AMAZING DISCOUNT
PLACE THIS ORDER OR A SIMILAR ORDER WITH ALL NURSING ASSIGNMENTS TODAY AND GET AN AMAZING DISCOUNT







